Fecal calprotectin is associated with disease activity in patients with ankylosing spondylitis
DOI:
https://doi.org/10.17305/bjbms.2016.752Keywords:
ankylosing spondylitis, calprotectin, disease activity, BASDAI, BASFIAbstract
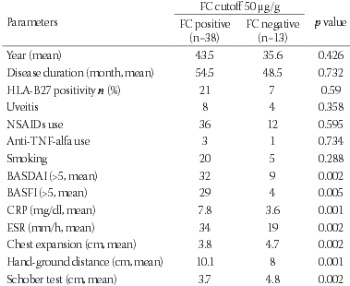
Calprotectin is one of the major antimicrobial S100 leucocyte proteins. Serum calprotectin levels are associated with certain inflammatory diseases such as rheumatoid arthritis, systemic lupus erythematosus and inflammatory bowel disease. The aim of this study was to investigate serum and fecal calprotectin levels in patients with ankylosing spondylitis (AS) and show their potential relations to the clinical findings of the disease. Fifty-one patients fulfilling the New York criteria of AS and 43 healthy age- and gender-matched volunteers were included in the study. Physical and locomotor system examinations were performed and history data were obtained for all patients. Disease activity parameters were assessed together with anthropometric parameters. Routine laboratory examinations and genetic testing (HLA-B27) were performed. Serum calprotectin levels and fecal calprotectin levels were measured by an enzyme-linked immunosorbent assay. The mean age of the patients was 41.5 years, the mean duration of the disease was 8.6 years, and the delay in diagnosis was 4.2 years. Serum calprotectin levels were similar in both AS patients and in the control group (p=0.233). Serum calprotectin level was correlated with Bath AS disease activity index (BASDAI) and Bath AS functional index (BASFI) (p=0.001, p=0.002, respectively). A higher level of fecal calprotectin was detected in AS patients when compared with the control group. A statistically significant correlation between fecal calprotectin level and BASDAI, BASFI, C-reactive protein and Erythrocyte sedimentation rate were detected (p=0.002, p=0.005, p=0.001, p=0.002, respectively). The results indicated that fecal calprotectin levels were associated with AS disease findings and activity parameters. Calprotectin is a vital disease activity biomarker for AS and may have an important role in the pathogenesis of the disease. Multi-centered prospective studies are needed in order to provide further insight.
Citations
Downloads
References
Montalto M, Gallo A, Santoro L, D'Onofrio F, Landolfi R, Gasbarrini A. Role of fecal calprotectin in gastrointestinal disorders. Eur Rev Med Pharmacol Sci. 2013;17(12):1569–82.
. Hetland G, Talgö GJ, Fagerhol MK. Chemotaxins C5a and fMLP induce release of calprotectin (leucocyte L1 protein) from polymorphonuclear cells in vitro. Mol Pathol. 1998;51(3):143–8.
http://dx.doi.org/10.1136/mp.51.3.143
. Mielants H, Veys EM, Goemaere S, Goethals K, Cuvelier C, De Vos M. Gut inflammation in the spondyloarthropathies: clinical, radiologic, biologic and genetic features in relation to the type of histology. A prospective study. J Rheumatol 2015 Apr 16;18(10):1542–51.
. Rudwaleit M, Baeten D. Ankylosing spondylitis and bowel disease. Best Pract Res Clin Rheumatol. 2006;20(3):451–71.
http://dx.doi.org/10.1016/j.berh.2006.03.010
. Costello ME, Elewaut D, Kenna TJ, Brown M . Microbes, the gut and ankylosing spondylitis. Arthritis Res Ther 2013;15(3):214.
http://dx.doi.org/10.1186/ar4228
. Vermeire S, Van Assche G, Rutgeerts P. Laboratory markers in IBD: useful, magic, or unnecessary toys? Gut 2006;55(3):426–31.
http://dx.doi.org/10.1136/gut.2005.069476
. Osipenko MF, Livzan MA, Skalinskaia MI, Lialiukova EA. Fecal calprotectin concentration in the differential diagnosis of bowel diseases. Ter Arkh 2015;87(2):30–3.
. Mariani A, Marsili M, Nozzi M, Faricelli R, Chiarelli F, Breda L. Serum calprotectin: review of its usefulness and validity in paediatric rheumatic diseases. Clin Exp Rheumatol 2014;33(1):109–14.
. Wassell J, Wallage M, Brewer E. Evaluation of the Quantum Blue(R) rapid test for faecal calprotectin. Ann Clin Biochem. 2012;49(1):55–8.
http://dx.doi.org/10.1258/acb.2011.011106
. Oktayoglu P, Bozkurt M, Mete N, Caglayan M, Em S, Nas K. Elevated serum levels of calprotectin (myeloid-related protein 8/14) in patients with ankylosing spondylitis and its association with disease activity and quality of life. J Investig Med 2014;62(6):880–4.
http://dx.doi.org/10.1097/JIM.0000000000000095
. Klingberg E, Carlsten H, Hilme E, Hedberg M, Forsblad-d'Elia H. Calprotectin in ankylosing spondylitis – frequently elevated in feces, but normal in serum. Scand J Gastroenterol. 2012;47(4):435–44.
http://dx.doi.org/10.3109/00365521.2011.648953
. Matzkies FG, Targan SR, Berel D, Landers CJ, Reveille JD, McGovern DP, et al. Markers of intestinal inflammation in patients with ankylosing spondylitis: a pilot study. Arthritis Res Ther 2012;14(6):R261
http://dx.doi.org/10.1186/ar4106
. Turina M, Sieper J, Yeremenko N, Conrad K, Haibel H, Rudwaleit M, et al. Calprotectin serum level is an independent marker for radiographic spinal progression in axial spondyloarthritis. Ann Rheum Dis 2014;73:1746–1748.
http://dx.doi.org/10.1136/annrheumdis-2014-205506
. Dávida L, Szántó S, Kacska S, Haraszti B, Brúgós B, Altorjay I, et al. The role of fecal calprotectin in the prediction of ankylosing spondylitis associated with early IBD. J Crohns Colitis 2015;9 Suppl 1:S108–9.
http://dx.doi.org/10.1093/ecco-jcc/jju027.182
. Turina MC, Yeremenko N, Paramarta JE, De Rycke L, Baeten D. Calprotectin (S100A8/9) as serum biomarker for clinical response in proof-of-concept trials in axial and peripheral spondyloarthritis. Arthritis Res Ther. 2014;16(4):413.
http://dx.doi.org/10.1186/s13075-014-0413-4
. Manz M, Burri E, Rothen C, Tchanguizi N, Niederberger C, Rossi L, et al. Value of fecal calprotectin in the evaluation of patients with abdominal discomfort: an observational study. BMC Gastroenterol 2012;12(1):5.
http://dx.doi.org/10.1186/1471-230X-12-5
. Smith J. Update on Ankylosing Spondylitis: Current Concepts in Pathogenesis. Curr Allergy Asthma Rep 2014;15(1).
. Rashid T, Wilson C, Ebringer A. The link between ankylosing spondylitis, Crohn's disease, Klebsiella, and starch consumption. Clin Dev Immunol 2013 Jan;2013:872632.
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2015-10-26
Published 2016-01-01