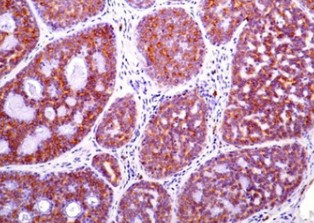
Role and significance of c-KIT receptor tyrosine kinase in cancer: A review
DOI:
https://doi.org/10.17305/bjbms.2021.7399Keywords:
c-KIT, CD117, cancer, receptor tyrosine kinases, stem cell factor receptorAbstract
c-kit is a classical proto-oncogene that encodes a receptor tyrosine kinase (RTK) that responds to stem cell factor (SCF). C-KIT signaling is a critical regulator of cell proliferation, survival, and migration and is implicated in several physiological processes, including pigmentation, hematopoiesis and gut movement. Accumulating evidence suggests that dysregulated c-KIT function, caused by either overexpression or mutations in c-kit, promotes tumor development and progression in various human cancers. In this review, we discuss the most important structural and biological features of c-KIT, as well as insights into the activation of intracellular signaling pathways following SCF binding to this RTK. We then illustrate how different c-kit alterations are associated with specific human cancers and describe recent studies that highlight the contribution of c-KIT to cancer stemness, epithelial-mesenchymal transition and progression to metastatic disease in different experimental models. The impact of tyrosine kinase inhibitors in treating c-KIT-positive tumors and limitations due to their propensity to develop drug resistance are summarized. Finally, we appraise the potential of novel therapeutic approaches targeting c-KIT more selectively while minimizing toxicity to normal tissue.
Citations
Downloads
Downloads
Additional Files
Published
License
Copyright (c) 2022 Emana Sheikh, Tony Tran, Semir Vranic, Arkene Levy, R. Daniel Bonfil

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2022-04-21
Published 2022-09-16