Associations of non-HDL-C and triglyceride/HDL-C ratio with coronary plaque burden and plaque characteristics in young adults
DOI:
https://doi.org/10.17305/bjbms.2022.7142Keywords:
non-high-density lipoprotein cholesterol, triglyceride/high-density lipoprotein cholesterol ratio, coronary plaque characteristic, coronary computed tomography angiographyAbstract
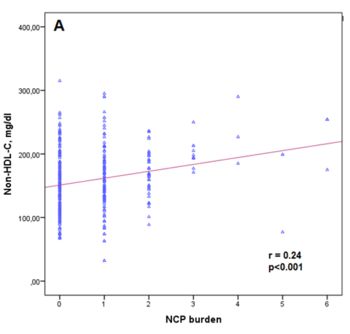
Coronary artery disease (CAD) is uncommon in young adult patients. However, these patients have different risk factor profiles and high-risk coronary plaques are more common. The aim of this study was to examine the relations between the coronary plaque burden, plaque composition, serum non-high-density lipoprotein cholesterol (non–HDL-C) levels, and triglyceride/high-density lipoprotein cholesterol (TG/HDL-C) ratio in young adults. We analyzed a total of 551 patients under age 45 who had undergone coronary computed tomography angiography (CCTA). Coronary plaque characteristics were analyzed using CCTA. Multivariate linear regression analysis was used to assess the predictors of non-calcified plaque (NCB) and calcified plaque (CB) burdens. Serum non–HDL-C levels and TG/HDL-C ratio were higher in the coronary atherosclerosis patient group. Serum non–HDL-C levels and the TG/HDL-C ratio were higher in the obstructive CAD patient group. The plaque burden was positively correlated with non-HDL-C (r = 0.30; p < 0.001), and TG/HDL-C ratio (r = 0.18; p < 0.001). NCB was positively correlated with age, gender, smoking status, fasting blood glucose, total cholesterol, low-density lipoprotein cholesterol, serum triglycerides, hbA1c, non–HDL-C, and TG/HDL-C ratio. Non–HDL-C (β coefficient = 0.13; p = 0.023) and TG/HDL-C ratio (β = 0.10; p = 0.042) were independent predictors of NCB. Serum non–HDL-C levels and TG/HDL-C were significantly associated with the presence and burden of coronary plaques. Serum non–HDL-C and TG/HDL-C ratios were independently associated with NCB, suggesting their use as easy-to-compute markers for identifying high-risk groups in young adults.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2022 Fatih Akin, İbrahim Altun, Burak Ayca, Nuri Kose, İlknur Altun

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2022-04-26
Published 2022-10-23









