Untangling the relationship between hemoglobin, peak troponin level, and mortality in patients with myocardial infarction
DOI:
https://doi.org/10.17305/bjbms.2021.6744Keywords:
baseline hemoglobin, myocardial infarction, myocardial injury, infarct size, percutaneus coronary intervention, body surface area, outcome, mortalityAbstract
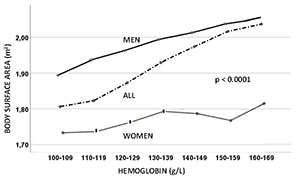
Patients with a history of myocardial infarction (MI) and lower admission hemoglobin (aHb) levels have a worse outcome than patients with higher aHb, but lower or similar peaks in enzymatic infarct size. Hemoglobin levels are positively correlated with body surface area (BSA), which is positively correlated with cardiac mass. We hypothesized that patients with lower aHb suffer comparatively greater myocardial injury. We examined the relationships between aHb, and troponin (Tn) normalized to BSA (Tn/BSA) and its association with 30-day mortality. Data from 6055 patients, who were divided into seven groups based on their aHb at 10g/L intervals, were analyzed, and the groups were compared. The relationships between aHb and Tn/BSA and between Tn/BSA and 30-day mortality were assessed. Patients with higher aHb levels had greater BSA (p<0.0001). A negative relationship between aHb and log10Tn/BSA was observed in the entire group, and in men and women separately (p<0.0001, p<0.0001, and p=0.013, respectively). The log10Tn/BSA value was associated with 30-day mortality in the entire group, and in men and women separately (p<0.0001, p=0.014, and p<0.0001, respectively). Our finding suggests that a similar peak Tn value in patients with lower aHb means comparatively greater myocardial injury relative to cardiac mass. This hypothesis helps to explain the worse outcomes in patients with lower aHb. According to our findings, troponin should be indexed to BSA to provide comparable information on cardiac injury relative to cardiac mass. Whether this relationship is causal remains to be clarified.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2022 Vojko Kanic, Gregor Kompara, David Suran, Nina Glavnik Poznic

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2022-02-08
Published 2022-09-16









