Impact of smoking on the incidence and post-operative complications of total knee arthroplasty: A systematic review and meta-analysis of cohort studies
DOI:
https://doi.org/10.17305/bjbms.2021.6538Keywords:
Total Knee Arthroplasty, Smoking, Incidence, ComplicationsAbstract
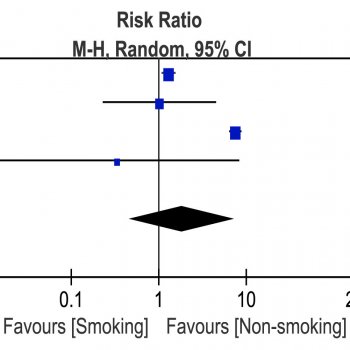
Osteoarthritis and rheumatoid arthritis are the most ubiquitous joint disorders which cause tremendous loss of life quality and impose an economic burden on society. At present, the treatment options for these two diseases comprise non-operative and surgical treatments, amongst those total knee arthroplasties (TKA). Various studies have recognized smoking as a significant risk factor for postoperative complications. Therefore, the purpose of this study was to examine the impact of smoking on the incidence and postoperative complications after a total knee arthroplasty by a systematic review and meta-analysis. The research was performed using PUBMED, Cochrane Library and EMBASE, extracting data from thirteen suitable studies and incorporating 2,109,482 patients. Cohort studies evaluating the impact of smoking on TKA with sufficient data were included for the study, and cohort studies without a proper control group and complete data were excluded. A fixed-effects or random-effects model was used to measure the pooled risk ratio (RR) or hazard ratio (HR) with 95% confidence interval (CI). Compared to non-smokers, smokers had a significantly lower incidence of TKA (p<0.01). However, smokers had a higher incidence of total complications (p=0.01), surgical complications (p<0.01), pneumonia (p<0.01) and revision surgery (p=0.01). No significant difference in the risk of blood transfusion (p=0.42), deep vein thrombosis (p=0.31), pulmonary embolism (p=0.34), urinary tract infection (p=0.46) or mortality (p=0.39) was found between smokers and non-smokers. In conclusion, the study indicated that tobacco has two diametrically opposite effects on TKA patients: 1. Tobacco increases the incidence of surgical complications, pneumonia and revision after TKA; 2. It decreases the overall risk of being a candidate for TKA.
Citations
Downloads
Downloads
Additional Files
Published
License
Copyright (c) 2021 Yuqi He, Mohamed Omar, Xiaoyuan Feng, Claudia Neunaber, Michael Jagodzinski

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2021-11-05
Published 2022-06-01









