Impacts of N-Butylphthalide on expression of growth factors in rats with focal cerebral ischemia
DOI:
https://doi.org/10.17305/bjbms.2016.560Keywords:
N-butylphthalide, rats with cerebral ischemia and reperfusion, vascular endothelial growth factor, transforming growth factor-β1Abstract
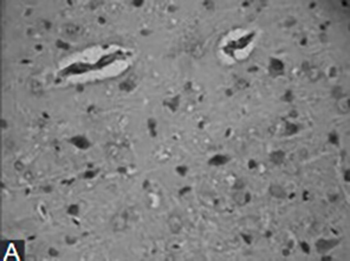
This study investigates the impacts of n-butylphthalide (NBP) on the expression of vascular endothelial growth factor (VEGF) and transforming growth factor-β1 (TGF-β1) in rats with focal cerebral ischemia. The thread embolization method was used to prepare the rat model of cerebral ischemia-reperfusion (CIR). The animals were divided into a sham operation group, a model control group and NBP treatment group. The NBP group was orally administered 25 mg/kg NBP twice a day after the surgery. The immunohistochemistry and reverse transcription-polymerase chain reaction were performed to observe the protein and mRNA expressions of VEGF and TGF-β 16 hours, 1 day and 2 days after inducing CIR. The mRNA and protein expressions of VEGF and TGF-β1 in the model control group and the NBP treatment group were all increased after CIR, and those of the NBP treatment group at each post-CIR time point were higher than the model control group (p < 0.01). After CIR, the expressions of VEGF and TGF-β1 increased, suggesting that VEGF and TGF-β1 exhibited protective effects towards the ischemic brain injuries, and that NBP could upregulate the expressions of VEGF and TGF-β1 in the peri-infarcted area, thus possibly protecting the ischemic brain tissues through this mechanism.
Citations
Downloads
References
Tuor UI, Morgunov M, Sule M, Qiao M, Clark D, Rushforth D, et al. Cellular correlates of longitudinal diffusion tensor imaging of axonal degeneration following hypoxic-ischemic cerebral infarction in neonatal rats. Neuroimage Clin 2014;6:32-42. http://dx.doi.org/10.1016/j.nicl.2014.08.003.
Ferrara N, Henzel WJ. Pituitary follicular cells secrete a novel heparin-binding growth factor specific for vascular endothelial cells. Biochem Biophys Res Commun 1989;161(2):851-8. http://dx.doi.org/10.1016/0006-291X(89)92678-8.
Won S, Lee JH, Wali B, Stein DG, Sayeed I. Progesterone attenuates hemorrhagic transformation after delayed tPA treatment in an experimental model of stroke in rats: Involvement of the VEGF-MMP pathway. J Cereb Blood Flow Metab 2014;34(1):72-80. http://dx.doi.org/10.1038/jcbfm.2013.163.
Tang Y, Wang J, Lin X, Wang L, Shao B, Jin K, et al. Neural stem cell protects aged rat brain from ischemia-reperfusion injury through neurogenesis and angiogenesis. J Cereb Blood Flow Metab 2014;34(7):1138-47. http://dx.doi.org/10.1038/jcbfm.2014.61.
Cui W, Li W, Han R, Mak S, Zhang H, Hu S, et al. PI3-K/Akt and ERK pathways activated by VEGF play opposite roles in MPP-induced neuronal apoptosis. Neurochem Int 2011;59(6):945-53. http://dx.doi.org/10.1016/j.neuint.2011.07.005.
Ponce CC, de Lourdes Lopes Ferrari Chauffaille M, Ihara SS, Silva MR. Increased angiogenesis in primary myelofibrosis: Latent transforming growth factor-ß as a possible angiogenic factor. Rev Bras Hematol Hemoter 2014;36(5):322-8. http://dx.doi.org/10.1016/j.bjhh.2014.07.010.
Causey MW, Salgar S, Singh N, Martin M, Stallings JD. Valproic acid reversed pathologic endothelial cell gene expression profile associated with ischemia-reperfusion injury in a swine hemorrhagic shock model. J Vasc Surg 2012;55(4):1096-1103.e51. http://dx.doi.org/10.1016/j.jvs.2011.08.060.
Goumans MJ, Lebrin F, Valdimarsdottir G. Controlling the angiogenic switch: A balance between two distinct TGF-b receptor signaling pathways. Trends Cardiovasc Med 2003;13(7):301-7. http://dx.doi.org/10.1016/S1050-1738(03)00142-7.
Thored P, Wood J, Arvidsson A, Cammenga J, Kokaia Z, Lindvall O. Long-term neuroblast migration along blood vessels in an area with transient angiogenesis and increased vascularization after stroke. Stroke 2007;38(11):3032-9. http://dx.doi.org/10.1161/STROKEAHA.107.488445.
Li Y, Lu Z, Keogh CL, Yu SP, Wei L. Erythropoietin-induced neurovascular protection, angiogenesis, and cerebral blood flow restoration after focal ischemia in mice. J Cereb Blood Flow Metab 2007;27(5):1043-54.
Longa EZ, Weinstein PR, Carlson S, Cummins R. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 1989;20(1):84-91. http://dx.doi.org/10.1161/01.STR.20.1.84.
Zausinger S, Hungerhuber E, Baethmann A, Reulen H, Schmid-Elsaesser R. Neurological impairment in rats after transient middle cerebral artery occlusion: A comparative study under various treatment paradigms. Brain Res 2000;863(1-2):94-105. http://dx.doi.org/10.1016/S0006-8993(00)02100-4.
Greenberg DA, Jin K. Vascular endothelial growth factors (VEGFs) and stroke. Cell Mol Life Sci 2013;70(10):1753-61. http://dx.doi.org/10.1007/s00018-013-1282-8.
Yang ZJ, Bao WL, Qiu MH, Zhang LM, Lu SD, Huang YL, et al. Role of vascular endothelial growth factor in neuronal DNA damage and repair in rat brain following a transient cerebral ischemia. J Neurosci Res 2002;70(2):140-9. http://dx.doi.org/10.1002/jnr.10380.
Manoonkitiwongsa PS, Schultz RL, McCreery DB, Whitter EF, Lyden PD. Neuroprotection of ischemic brain by vascular endothelial growth factor is critically dependent on proper dosage and may be compromised by angiogenesis. J Cereb Blood Flow Metab 2004;24(6):693-702. http://dx.doi.org/10.1097/01.WCB.0000126236.54306.21.
Hansen TM, Moss AJ, Brindle NP. Vascular endothelial growth factor and angiopoietins in neurovascular regeneration and protection following stroke. Curr Neurovasc Res 2008;5(4):236-45. http://dx.doi.org/10.2174/156720208786413433.
Kim YH, Ryu JM, Lee YJ, Han HJ. Fibronectin synthesis by high glucose level mediated proliferation of mouse embryonic stem cells: Involvement of ANG II and TGF-beta1. J Cell Physiol 2010;223(2):397-407. http://dx.doi.org/10.1002/jcp.22048.
Ng J. TGF-beta signals regulate axonal development through distinct Smad-independent mechanisms. Development 2008;135:4025-35. http://dx.doi.org/10.1242/dev.028209.
Sun J, Zhou W, Sha B, Yang Y. Ischemia induced neural stem cell proliferation and differentiation in neonatal rat involved vascular endothelial growth factor and transforming growth factor-beta pathways. Brain Dev 2010;32:191-200. http://dx.doi.org/10.1016/j.braindev.2009.01.004.
Shih SC, Ju M, Liu N, Mo JR, Ney JJ, Smith LE. Transforming growth factor beta1 induction of vascular endothelial growth factor receptor 1: Mechanism of pericyte-induced vascular survival in vivo. Proc Natl Acad Sci U S A 2003;100(26):15859-64. http://dx.doi.org/10.1073/pnas.2136855100.
Brionne TC, Tesseur I, Masliah E, Wyss-Coray T. Loss of TGF-beta 1 leads to increased neuronal cell death and microgliosis in mouse brain. Neuron 2003;40(6):1133-45. http://dx.doi.org/10.1016/S0896-6273(03)00766-9.
Peng Y, Xu SF, Wang L. Effects of chiral NBP on cerebral infarct volume due to transient focal cerebral ischemia. Chin J N Drugs J 2005;14:420-3.
Deng W, Feng Y. Effect of dl-3-n-butylphthalide on brain edema in rats subjected to focal cerebral ischemia. Chin Med Sci J 1997;12:102-6.
Downloads
Additional Files
Published
How to Cite
Accepted 2015-08-01
Published 2016-01-01









