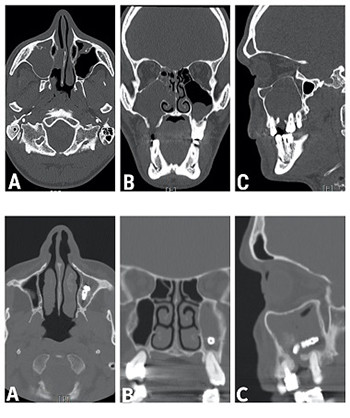
Chronic maxillary sinusitis of dental origin and oroantral fistula: The results of combined surgical approach in an Italian university hospital
DOI:
https://doi.org/10.17305/bjbms.2020.4748Keywords:
Chronic maxillary sinusitis of dental origin, oroantral fistula, odontogenic sinusitis, maxillary sinus disease, endoscopic sinus surgery, ostiomeatal complex, Lund- Mackay Grading, Rehrmann flapAbstract
Unilateral chronic maxillary sinusitis is a possible complication of odontogenic disease or dental treatment and is mainly due to the development of an oroantral fistula (OAF). The management of chronic maxillary sinusitis of dental origin (CMSDO) requires a combined treatment via endoscopic sinus surgery (ESS) and intraoral surgical treatment of the odontogenic source. The aim of this study is to present the results of our university hospital unit in the treatment and follow-up of a case series of 34 patients treated with a combined surgical approach for CMSDO due to OAF. All patients were treated with ESS combined with an intraoral approach. No intraoperative or immediate postoperative complications were observed; nasal synechia was found in 3 patients (8.82%). The overall success rate after the primary intervention was 94.12%; recurrence was observed in 2 cases (5.88%), both were suffering from diabetes mellitus and were tobacco smokers. Our results confirm that simultaneous surgery with a combination of an intraoral and endoscopic approach can be considered the best strategy for the long-term restoration of normal sinonasal homeostasis in selected patients with chronic odontogenic sinusitis and OAF, guaranteeing an effective treatment with minimal complications in the short and long term.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2020-04-29
Published 2020-11-02