Circulating long noncoding RNAs H19 and GAS5 are associated with type 2 diabetes but not with diabetic retinopathy: A preliminary study
DOI:
https://doi.org/10.17305/bjbms.2019.4533Keywords:
Long noncoding RNA, H19, GAS5, diabetic retinopathy, aflibercept, type 2 diabetes mellitus, T2DMAbstract
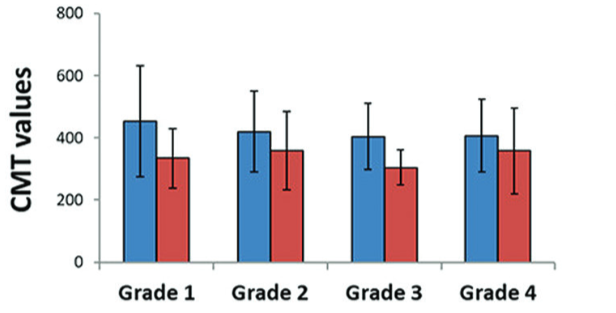
Recently, a wide range of biological and pathological roles of long noncoding RNAs (lncRNAs) have been discovered. However, the potential role of circulating lncRNAs H19 and GAS5 in type 2 diabetes mellitus (T2DM) and diabetic retinopathy (DR) is not clear. Here, we assessed the plasma levels of H19 and GAS5 lncRNAs in T2DM patients with/without DR and evaluated if H19 and GAS5 pre-treatment plasma levels are a predictor of early response to a single aflibercept dose in DR subgroup. Plasma lncRNA expression profiles of 119 T2DM patients (66 with DR and 53 without DR) and 110 healthy controls were determined by quantitative reverse transcription PCR. The association of lncRNA expression profiles with clinical features and aflibercept early response in DR patients was investigated. Relative H19 expression levels were significantly increased in T2DM group (including DR and non-DR subgroups) vs. controls, while GAS5 levels were decreased in T2DM group (p < 0.001). There was no significant difference in H19 and GAS5 expression levels between DR and non-DR subgroups. H19 and GAS5 expression profiles were not significantly correlated with clinical parameters or response to aflibercept therapy in DR subgroup. Our findings indicate that the circulating lncRNAs H19 and GAS5 may be associated with T2DM prevalence but may not have an important diagnostic/prognostic role in DR or early response to aflibercept intravitreal injection in DR patients. Large-scale transcriptomic studies are warranted to validate our results and investigate other lncRNA candidates in T2DM.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2020 Manal S. Fawzy, Ahmed A. Abdelghany , Eman A. Toraih

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2019-12-14
Published 2020-08-03









