Imaging Characteristics of Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leucoencephalopathy (CADASIL)
DOI:
https://doi.org/10.17305/bjbms.2015.247Keywords:
CADASIL, MRI, computed tomography, white matter hyperintensities, cerebral microbleedsAbstract
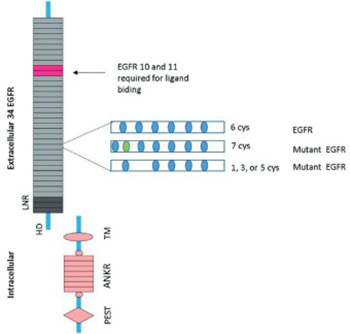
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leucoencephalopathy (CADASIL) is an autosomal dominant vascular disorder. Diagnosis and follow-up in patients with CADASIL are based mainly on magnetic resonance imaging (MRI). MRI shows white matter hyperintensities (WMHs), lacunar infarcts and cerebral microbleeds (CMBs). WMHs lesions tend to be symmetrical and bilateral, distributed in the periventricular and deep white matter. The anterior temporal lobe and external capsules are predilection sites for WMHs, with higher specificity and sensitivity of anterior temporal lobe involvement compared to an external capsule involvement. Lacunar infarcts are presented by an imaging signal that has intensity of cerebrospinal fluid in all MRI sequences. They are localized within the semioval center, thalamus, basal ganglia and pons. CMBs are depicted as focal areas of signal loss on T2 images which increases in size on the T2*-weighted gradient echo planar images (“blooming effect”).
Citations
Downloads
References
Desmond DW, Moroney JT, Lynch T, Chan S, Chin SS, Mohr JP. The natural history of CADASIL: a pooled Analysis of previously published cases. Stroke 1999;30(6):1230-1233.
http://dx.doi.org/10.1161/01.STR.30.6.1230
Opherk C, Peters N, Herzog J, Luedtke R, Dichgans M. Long term prognosis and causes of death in CADASIL: a retrospective study in 411 patients. Brain 2004;127(11):2533-2539.
http://dx.doi.org/10.1093/brain/awh282
Kalaria RN, Viitanen M, Kanlimo H, Dichagens M, Tabira T. The pathogenesis of CADASIL: an update. J Neurol Sci 2004;226(1-2):35-39.
http://dx.doi.org/10.1016/j.jns.2004.09.008
Chabriat H. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Geriatr Psychol Neuropsychiatr Vieil 2014;12(2):183-192.
Peters N, Opherk C, Danek A, Ballard C, Herzog J, Dichgans M. The pattern of cognitive performance in CADASIL: a monogenic condition leading to subcortical ischemic vascular dementia. Am J Psychiatry 2005;162(11):2078-2085.
http://dx.doi.org/10.1176/appi.ajp.162.11.2078
Kim YE, Yoon CW, Seo SW, Ki CS, Kim YB, Kim JW, et al. Spectrum of NOTCH3 mutations in Korean patients with clinically suspicious cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Neurobiol Aging 2014;35(3):726.e1-6.
Razvi SS, Davidson R, Bone I, Muir KW. The prevalence of cerebral autosomal-dominant arteriopathy with subcortical infarcts and leucoencephalopathy (CADASIL) in the west of Scotland. J Neurol Neurosurg Psychiatry 2005;76(5):739-741.
http://dx.doi.org/10.1136/jnnp.2004.051847
Joutel A, Corperchot C, Ducros A, Vahedi K, Chabriat H, Mouton P, et al. Notch3 mutation in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature 1996;383(6602):707-710.
http://dx.doi.org/10.1038/383707a0
Bianchi S, Zicari E, Carluccio A, Di Donato I, Pescini F, Nannucci S, et al. CADASIL in central Italy: a retrospective clinical and genetic study in 229 patients. J Neurol 2015;262(1):134-141.
http://dx.doi.org/10.1007/s00415-014-7533-2
Rutten JW, Haan J, Terwindt GM, van Duinen SG, Boon EM, Lesnik Oberstein SA. Interpretation of NOTCH3 mutations in the diagnosis of CADASIL. Expert Rev Mol Diagn 2014;14(5):593-603.
http://dx.doi.org/10.1586/14737159.2014.922880
Zea-Sevilla MA, Bermejo-Velasco P, Serrano-Heranz R, Calero M. Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy (CADASIL) associated with a Novel C82R Mutation in the NOTCH3 Gene. J Alzheimers Dis 2015;43(2):363-367.
Herve D, Chabriat H. CADASIL. J Geriatr psychiatry Neurol 2010;23(4):269-276.
http://dx.doi.org/10.1177/0891988710383570
Lee YC, Liu CS, Chang MS, Lin KP, Fuh JL, Lu YC, et al. Population-specific spectrum of NOTCH3 mutations, MRI features and founder effect of CADASIL in Chinese. J Neurol 2009;256(2):249-255.
http://dx.doi.org/10.1007/s00415-009-0091-3
Mignarri A, Martini G, Malandrini A, Bellini M, Bianchi S, Tassi R, et al. First report of Iraqi Kurdish CADASIL patient. NeurolSci 2011;32(2):359-360.
http://dx.doi.org/10.1007/s10072-010-0399-x
Federico A, Bianchi S, Dotti MT. The spectrum of mutations for CADASIL diagnosis. Neurol Sci 2005;26(2):117-124.
http://dx.doi.org/10.1007/s10072-005-0444-3
Stojanov D, Grozdanovic D, Petrovic S, Benedeto-Stojanov D, Stefanovic I, Stojanovic N, et al. De novo mutation in the NOTCH3 gene causing CADASIL. Bosn J Basic Med Sci 2014;14(1):48-50.
Joutel A, Dodick DD, Parisi JE, Cecillon M, Tournier-Lasserve E, Bousser MG. De novo mutation in the Notch3 gene causing CADASIL. Ann Neurol 2000;47(3):388-391.
http://dx.doi.org/10.1002/1531-8249(200003)47:3<388::AID-ANA19>3.0.CO;2-Q
Coto E, Menéndez M, Navarro R,Garcia-Castro M, Alvarez V. A new de novo Notch3 mutation causing CADASIL. Eur J Neurol 2006;13(6):628-631.
http://dx.doi.org/10.1111/j.1468-1331.2006.01337.x
Yamamoto Y, Ihara M, Tham C, Low RW, Slade JY, Moss T, et al. Neuropathological correlates of temporal white matter hyperintensities in CADASIL. Stroke 2009;40(6):2004-2011.
http://dx.doi.org/10.1161/STROKEAHA.108.528299
Yamamoto Y, Craggs LJ, Watanabe A, Booth T, Attems J, Low RW. Brain microvascular accumulation and distribution of the NOTCH3 ectodomain and granular osmiophilic material in CADASIL. J Neuropathol Exp Neurol 2013;72(5):416-431.
http://dx.doi.org/10.1097/NEN.0b013e31829020b5
Uchino M. The pathomechanism and treatment of CADASIL. Rinsho Shinkeiqaku 2011;51(11):945-948.
http://dx.doi.org/10.5692/clinicalneurol.51.945
Peisker T, Musli L, Hrebicek M, Vlaskova H, Cihelkova I, Bartos A. Clinical spectrum in CADASIL family with a new mutation. Biomed Pup Med Fac Univ Palacky Olomouc Czech Rep 2013;157(4):379-382. doi: 10.5507/bp.2013.055.
http://dx.doi.org/10.5507/bp.2013.055
Choudhary S, McLeod M, Torchia D, Romanelli P. Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy (CADASIL). J Clin Aesthet Dermatol 2013;6(3):29-33.
Lee JS, Choi JC, Kang SY, Kang JH, Na HR, Park JK. Effects of lacunar infarctions on cognitive impairment in patients with cerebral autosomal-dominant arteriopathy with subcortical infarcts and leucoencephalopathy. J Clin Neurol 2011;7(4):210-214.
http://dx.doi.org/10.3988/jcn.2011.7.4.210
Singhal S, Rich R, Markus HS. The spatial distribution of MR image abnormalities in cerebral autosomal-dominant arteriopathy with subcortical infarcts and leucoencephalopathy and their relationship to age and clinical features. Am J Neuroradiol 2005;26(10):2481-2487.
vanden Boom R, Lesnik Oberstein SA, Ferrari MD, Haan J, van Buchem MA.Cerebral autosomal-dominant arteriopathy with subcortical infarcts and leucoencephalopathy: MRI imaging findings at different ages – 3rd-6th decades. Radiology 2003;229(3):683-690.
http://dx.doi.org/10.1148/radiol.2293021354
Lesnik Oberstein SA, van den Boom R, van Buchem MA,van Houwelingen HC, Bakker E, Vollebregt E, et al.Cerebral microbleeds in CADASIL. Neurology 2001;57(6):1066-1070.
http://dx.doi.org/10.1212/WNL.57.6.1066
Choi JC. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leucoencephalopathy: a genetic cause of cerebral small vesels disease. J Clin Neurol 2010;6(1):1-9.
http://dx.doi.org/10.3988/jcn.2010.6.1.1
Bender B, Bornemann A, Reimold M, Ernemann U, Horger M. Imaging findings in autosomal-dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) - CADASIL - the most frequent familial stroke syndrome. Rofo 2012;184(8):679-683.
http://dx.doi.org/10.1055/s-0032-1318829
Aracki-Trenkic A, Stojanov D. Imaging characteristics of CADASIL patient with inherited and de novo gene NOTCH 3Q19 mutation. [Accessed 10 October 2014] Retrieved from: http://posterng.netkey.at/esr/viewing/index.php?module=viewing_poster&doi=10.1594/ecr2014/C-0309. http://dx.doi.org/10.1594/ecr2014/C-0309
Chabriat H, Levy C, Taillia H, Iba-Zizen MT, Vahedi K, Joutel A, et al. Patterns of MRI lesions in CADASIL. Neurology 1998;51(2):452-457.
http://dx.doi.org/10.1212/WNL.51.2.452
Benisty S, Reyes S, Godin O, Hervé D, Zieren N, Jouvent E, et al. White-matter lesions without lacunar infarcts in CADASIL. Alzheimers Dis 2012;29(4):903-911. DOI:10.3233/JAD-2012-111784
Skehan SJ, Hutchinson M, MacErlaine DP. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leucoencephalopathy: MR findings. AJNR Am J Neuroradiol 1995;16(10):2115-2119.
Coulthard A, Blank S, Bushby K, Kalaria RN, Burn DJ. Distribution of cranial MRI abnormalities in patients with symptomatic and subclinical CADASIL. Br J Radiol 2000;73(867):256-265.
http://dx.doi.org/10.1259/bjr.73.867.10817040
De Guio F, Mangin JF, Duering M, Ropele S, Chabriat H, Jouvent E. White Matter Edema at the Early Stage of Cerebral Autosomal-Dominant Arteriopathy With Subcortical Infarcts and Leukoencephalopathy. Stroke 2015;46(1):258-261.
http://dx.doi.org/10.1161/STROKEAHA.114.007018
O'Sullivan M, Jarosz JM, Martin RJ, Deasy N, Powell JF, Markus HS. MRI hyperintensities in the temporal lobe and external capsule in patients with CADASIL. Neurology 2001;56(5):628-634.
http://dx.doi.org/10.1212/WNL.56.5.628
Auer DP, Putz B, Gossl C, Elbel G, Gasser T, Dichgans M. Differential lesion patterns in CADASIL and sporadic subcortical arteriosclerotic encephalopathy: MR imaging study with statistical parametric group comparison. Radiology 2001;218(2):443-451.
http://dx.doi.org/10.1148/radiology.218.2.r01fe24443
Marcus HS, Martin RJ, Simpson MA, Dong YB, Ali N, Crosby AH, et al. Diagnostic strategies in CADASIL. Neurology 2002;59(8):1134-1138.
http://dx.doi.org/10.1212/WNL.59.8.1134
Kobayashi J, Sato S, Okumura K, Miyashita F, Ueda A, Ando Y, et al. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy without anterior temporal pole involvement: a case report. Stroke Cerebrovasc Dis 2014;23(3):e241-242.
http://dx.doi.org/10.1016/j.jstrokecerebrovasdis.2013.10.013
Hacinski V, Iadecola C, Petersen RC, Breteler MM, Nyenhuis DL, Black SE, et al. National Institute of Neurological Disorders and Stroke – Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke 2006;37(9):2220-2241.
http://dx.doi.org/10.1161/01.STR.0000237236.88823.47
Mendes Coelho VC, Bertholdo D, Ono SE, de Carvalho Neto A. MRI hydrographic 3D sequences in CADASIL. Neurology 2014;82(4):371.
http://dx.doi.org/10.1212/WNL.0000000000000056
Moody DM, Bell MA, Challa VR. The corpus callosum, a unique whitte-matter tract: anatomic features that may explain sparing in Binswanger disease and resistance to the flow of fluid masses. Am J Neuroradiol 1988;9(6):1051-1059.
De Guio F, Reyes S, Duering M, Pirpamer L, Chabriat H, Jouvent E. Decreased T1 contrast between gray matter and normal-appearing white matter in CADASIL. AJNR Am J Neuroradiol 2014;35(1):72-76.
http://dx.doi.org/10.3174/ajnr.A3639
Yao M, Hervé D, Jouvent E, Duering M, Reyes S, Godin O, et al. Dilated perivascular spaces in small-vessel disease: a study in CADASIL. Cerebrovasc Dis 2014;37(3):155-163.
http://dx.doi.org/10.1159/000356982
Bokura H, Kobayashi S, Yamaguchi S. Distinguishing silent lacunar infarctions from enlarged Virchow-Robin spaces: a magnetic resonance imaging and pathological study. J Neurol 1998;245(2):116-122.
http://dx.doi.org/10.1007/s004150050189
Koennecke HC. Cerebral microbleeds on MRI: prevalence, associations, and potential clinical implications.Neurology 2006;66(2):165-171.
http://dx.doi.org/10.1212/01.wnl.0000194266.55694.1e
Vitali P, Boghen D, Daneault N, Guillon-Létourneau L, Poppe AY. Cerebral microbleed causing an acute stroke-like episode in a CADASIL patient. Can J Neurol Sci 2014;41(5):661-663.
http://dx.doi.org/10.1017/cjn.2014.29
Oh SI, Kim SH, Kim HJ. Massive pontine microbleeds in a patient with CADASIL. JAMA Neurol 2014;71(8):1048-1049.
http://dx.doi.org/10.1001/jamaneurol.2014.45
De Guio F, Reyes S, Vignaud A, Duering M, Ropele S, Duchesnay E, et al. In vivo high-resolution 7 Tesla MRI shows early and diffuse cortical alterations in CADASIL. PLoS One 2014;9(8):e106311.
http://dx.doi.org/10.1371/journal.pone.0106311
Lian L, Li D, Xue Z, Liang Q, Xu F, Kang H, et al. Spontaneous intracerebral hemorrhage in CADASIL. J Headache Pain 2013;14:98.
http://dx.doi.org/10.1186/1129-2377-14-98
Rinnoci V, Nannucci S, Valenti R, Donnini I, Bianchi S, Pescini F, et al. Cerebral hemorrhages in CADASIL: report of four cases and a brief review. J Neurol Sci 2013;330(1-2):45-51.
http://dx.doi.org/10.1016/j.jns.2013.04.002
Schrag M, Greer DM. Clinical associations of cerebral microbleeds on magnetic resonance neuroimaging. J Stroke Cerebrovasc Dis 2014;23(10):2489-2497.
http://dx.doi.org/10.1016/j.jstrokecerebrovasdis.2014.07.006
Gunda B, Porcher R, Duering M, Guichard JP, Mawet J, Jouvent E, et al. ADC histograms from routine DWI for longitudinal studies in cerebral small vessel disease: a field study in CADASIL. PLoS One 2014;9(5):e97173.
http://dx.doi.org/10.1371/journal.pone.0097173
Holtmannspotter M, Peters N, Opherk C, Martin D, Herzog J, Brückmann H, et al. Diffusion magnetic resonance histograms as a surrogate marker and predictor of disease progression in CADASIL: a two-year follow-up study. Stroke 2005;36(12):2559-2565.
http://dx.doi.org/10.1161/01.STR.0000189696.70989.a4
Liem MK, Lesnik Oberstein SA, Versluis MJ, Maat-Schieman ML, Haan J, Webb AG, et al. 7 T MRI reveals diffuse iron deposition in putamen and caudate nucleus in CADASIL. J Neurol Neurosurg Psychiatry 2012;83(12):1180-1185.
http://dx.doi.org/10.1136/jnnp-2012-302545
Yamada K, Sakai K, Akazawa K, Sugimoto N, Nakagawa M, Mizuno T. Detection of early neuronal damage in CADASIL patients by q-space MR imaging. Neuroradiology 2013;55(3):283-290.
Downloads
Additional Files
Published
How to Cite
Accepted 2014-12-18
Published 2015-02-09









