Predictors and incidence of hospitalization due to respiratory syncytial virus (RSV)-associated lower respiratory tract infection (LRTI) in non-prophylaxed moderate-to-late preterm infants in Bosnia and Herzegovina
DOI:
https://doi.org/10.17305/bjbms.2018.2318Keywords:
Hospitalization, moderate-to-late preterm infants, respiratory syncytial virus, RSV, lower respiratory tract infection, LRTIAbstract
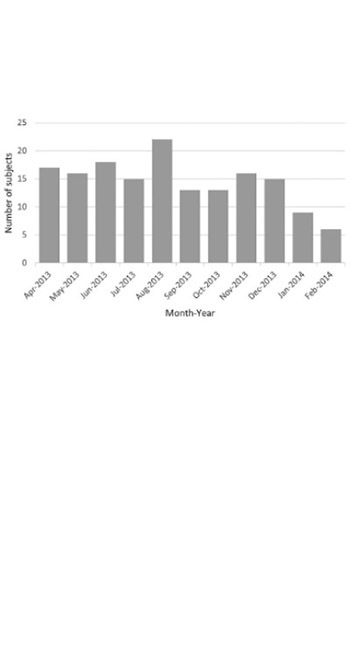
Prematurity is a risk factor for respiratory syncytial virus (RSV)-associated lower respiratory tract infections (LRTIs), due to immature humoral and cell-mediated immune system in preterm newborns, as well as their incomplete lung development. Palivizumab, a humanized monoclonal antibody against the F glycoprotein of RSV, is licensed for the prevention of severe RSV LRTI in children at high risk for the disease. This study is a part of a larger observational, retrospective-prospective epidemiological study (PONI) conducted at 72 sites across 23 countries in the northern temperate zone. The aim of our non-interventional study was to identify common predictors and factors associated with RSV LRTI hospitalization in non-prophylaxed, moderate-to-late preterm infants, born between 33 weeks and 0 days and 35 weeks and 6 days of gestation, and less than 6 months prior to or during the RSV season in Bosnia and Herzegovina (BH). A total of 160 moderate-to-late preterm infants were included from four sites in BH (Sarajevo, Tuzla, Mostar, and Banja Luka). We identified several significant intrinsic and extrinsic factors to be associated with the risk of RSV LRTI hospitalization in the preterm infants, including: comorbidities after birth, shorter hospital stay, admission to NICU/PICU while in the maternity ward, household smoking, low maternal age, breastfeeding, number of family members, and history of family/paternal atopy. Overall, our results indicated that the risk of RSV LRTI in preterm newborns can be associated with different environmental and social/cultural factors, and further research is needed to comprehensively evaluate these associations.
Citations
Downloads
References
Nair H, Nokes DJ, Gessner BD, Dherani M, Madhi SA, Singleton RJ, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: A systematic review and meta-analysis. Lancet 2010;375(9725):1545-55.
https://doi.org/10.1016/S0140-6736(10)60206-1.
Hall CB, Weinberg GA, Iwane MK, Blumkin AK, Edwards KM, Staat MA, et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med 2009;360(6):588-98. https://doi.org/10.1056/NEJMoa0804877.
Shay DK, Holman RC, Newman RD, Liu LL, Stout JW, Anderson LJ. Bronchiolitis-associated hospitalizations among US children, 1980-1996. JAMA 1999;282(15):1440-6. https://doi.org/10.1001/jama.282.15.1440.
Stockman LJ, Curns AT, Anderson LJ, Fischer-Langley G. Respiratory syncytial virus-associated hospitalizations among infants and young children in the United States, 1997-2006. Pediatr Infect Dis J 2012;31(1):5-9. https://doi.org/10.1097/INF.0b013e31822e68e6.
Glezen WP, Paredes A, Allison JE, Taber LH, Frank AL. Risk of respiratory syncytial virus infection for infants from low-income families in relationship to age, sex, ethnic group, and maternal antibody level. J Pediatr 1981;98(5):708-15.
https://doi.org/10.1016/S0022-3476(81)80829-3.
Groothuis JR, Levin MJ, Rodriguez W, Hall CB, Long CE, Kim HW, et al. Use of intravenous gamma globulin to passively immunize high-risk children against respiratory syncytial virus: Safety and pharmacokinetics. The RSVIG Study Group. Antimicrob Agents Chemother 1991;35(7):1469-73. https://doi.org/10.1128/AAC.35.7.1469.
Meissner HC, Fulton DR, Groothuis JR, Geggel RL, Marx GR, Hemming VG, et al. Controlled trial to evaluate protection of high-risk infants against respiratory syncytial virus disease by using standard intravenous immune globulin. Antimicrob Agents Chemother 1993;37(8):1655-8. https://doi.org/10.1128/AAC.37.8.1655.
Synagis. Synagis (palivizumab) injection. US Food & Drug Administration (FDA) approved product information. US National Library of Medicine; 2014.
Boyce TG, Mellen BG, Mitchel EF Jr, Wright PF, Griffin MR. Rates of hospitalization for respiratory syncytial virus infection among children in medicaid. J Pediatr 2000;137(6):865-70. https://doi.org/10.1067/mpd.2000.110531.
Kristensen K, Stensballe LG, Bjerre J, Roth D, Fisker N, Kongstad T, et al. Risk factors for respiratory syncytial virus hospitalisation in children with heart disease. Arch Dis Child 2009;94(10):785-9. https://doi.org/10.1136/adc.2008.143057.
Navas L, Wang E, de Carvalho V, Robinson J. Improved outcome of respiratory syncytial virus infection in a high-risk hospitalized population of Canadian children. Pediatric Investigators Collaborative Network on Infections in Canada. J Pediatr 1992;121(3):348-54. https://doi.org/10.1016/S0022-3476(05)90000-0.
Wang EE, Law BJ, Boucher FD, Stephens D, Robinson JL, Dobson S, et al. Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) study of admission and management variation in patients hospitalized with respiratory syncytial viral lower respiratory tract infection. J Pediatr 1996;129(3):390-5.
https://doi.org/10.1016/S0022-3476(96)70071-9.
Aurivillius M, Oymar K, Oxelius VA. Immunoglobulin heavy G2 chain (IGHG2) gene restriction in the development of severe respiratory syncytial virus infection. Acta Paediatr 2005;94(4):414-8. https://doi.org/10.1080/08035250410023656.
Welliver TP, Garofalo RP, Hosakote Y, Hintz KH, Avendano L, Sanchez K, et al. Severe human lower respiratory tract illness caused by respiratory syncytial virus and influenza virus is characterized by the absence of pulmonary cytotoxic lymphocyte responses. J Infect Dis 2007;195(8):1126-36. https://doi.org/10.1086/512615.
Del Vecchio A, Ferrara T, Maglione M, Capasso L, Raimondi F. New perspectives in Respiratory Syncitial Virus infection. J Matern Fetal Neonatal Med 2013;26(Suppl 2):55-9. https://doi.org/10.3109/14767058.2013.831282.
Cunningham CK, McMillan JA, Gross SJ. Rehospitalization for respiratory illness in infants of less than 32 weeks' gestation. Pediatrics 1991;88(3):527-32.
Stevens TP, Sinkin RA, Hall CB, Maniscalco WM, McConnochie KM. Respiratory syncytial virus and premature infants born at 32 weeks' gestation or earlier: Hospitalization and economic implications of prophylaxis. Arch Pediatr Adolesc Med 2000;154(1):55-61.
Gavin NI, Leader S. Predictive accuracy of risk factors for RSV-related hospitalizations among infants in low-income families born at 32 to 35 weeks of gestation. Journal of Clinical Outcomes Management 2007;14:323-31.
Blanken MO, Koffijberg H, Nibbelke EE, Rovers MM, Bont L, Dutch RSV Neonatal Network. Prospective validation of a prognostic model for respiratory syncytial virus bronchiolitis in late preterm infants: A multicenter birth cohort study. PLoS One 2013;8(3):e59161. https://doi.org/10.1371/journal.pone.0059161.
Straňák Z, Saliba E, Kosma P, Posfay-Barbe K, Yunis K, Farstad T, et al. Predictors of RSV LRTI hospitalization in infants born at 33 to 35 weeks gestational age: A large multinational study (PONI). PLoS One 2016;11(6):e0157446. https://doi.org/10.1371/journal.pone.0157446.
American Academy of Pediatrics. Respiratory syncytial virus. Red Book; 2012.
Report of the Committee on Infectious Diseases. American Academy of Pediatrics: Elk Grove Village, IL; 2012. p. 609.
Hall CB, Walsh EE, Long CE, Schnabel KC. Immunity to and frequency of reinfection with respiratory syncytial virus. J Infect Dis 1991;163(4):693-8. https://doi.org/10.1093/infdis/163.4.693.
World Health Organization. International statistical classification of diseases and related health problems (ICD-10). 10th revision. World Health Organization; 2010.
American Academy of Pediatrics (AAP), American College of Obstetricians and Gynecologists (ACOG). Guidelines for Perinatal Care. 7th ed; 2012.
Garcia CG, Bhore R, Soriano-Fallas A, Trost M, Chason R, Ramilo O, et al. Risk factors in children hospitalized with RSV bronchiolitis versus non-RSV bronchiolitis. Pediatrics 2010;126(6):e1453-60. https://doi.org/10.1542/peds.2010-0507.
Weisman L. Populations at risk for developing respiratory syncytial virus and risk factors for respiratory syncytial virus severity: Infants with predisposing conditions. Pediatr Infect Dis J 2003;22(2 Suppl):S33-7. https://doi.org/10.1097/01.inf.0000053883.08663.e5.
Meert K, Heidemann S, Abella B, Sarnaik A. Does prematurity alter the course of respiratory syncytial virus infection? Crit Care Med 1990;18(12):1357-9. https://doi.org/10.1097/00003246-199012000-00009.
Resch B, Gusenleitner W, Muller W. The impact of respiratory syncytial virus infection: A prospective study in hospitalized infants younger than 2 years. Infection 2002;30(4):193-7. https://doi.org/10.1007/s15010-002-2122-1.
Holman RC, Shay DK, Curns AT, Lingappa JR, Anderson LJ. Risk factors for bronchiolitis-associated deaths among infants in the United States. Pediatr Infect Dis J 2003;22(6):483-90. https://doi.org/10.1097/01.inf.0000069765.43405.3b.
Simoes EA, King SJ, Lehr MV, Groothuis JR. Preterm twins and triplets. A high-risk group for severe respiratory syncytial virus infection. Am J Dis Child 1993;147(3):303-6. https://doi.org/10.1001/archpedi.1993.02160270065020.
Yuksel B, Greenough A. Birth weight and hospital readmission of infants born prematurely. Arch Pediatr Adolesc Med 1994;148(4):384-8. https://doi.org/10.1001/archpedi.1994.02170040050008.
Hakulinen A, Heinonen K, Jokela V, Launiala K. Prematurity-associated morbidity during the first two years of life. A population-based study. Acta Paediatr Scand 1988;77(3):340-8. https://doi.org/10.1111/j.1651-2227.1988.tb10658.x.
Combs-Orme T, Fishbein J, Summerville C, Evans MG. Rehospitalization of very-low-birth-weight infants. Am J Dis Child 1988;142(10):1109-13. https://doi.org/10.1001/archpedi.1988.02150100103037.
Nachman SA, Navaie-Waliser M, Qureshi MZ. Rehospitalization with respiratory syncytial virus after neonatal intensive care unit discharge: A 3-year follow-up. Pediatrics 1997;100(6):E8. https://doi.org/10.1542/peds.100.6.e8.
Holberg CJ, Wright AL, Martinez FD, Ray CG, Taussig LM, Lebowitz MD. Risk factors for respiratory syncytial virus-associated lower respiratory illnesses in the first year of life. Am J Epidemiol 1991;133(11):1135-51. https://doi.org/10.1093/oxfordjournals.aje.a115826.
McConnochie KM, Roghmann KJ, Liptak GS. Hospitalization for lower respiratory tract illness in infants: Variation in rates among counties in New York State and areas within Monroe County. J Pediatr 1995;126(2):220-9.
https://doi.org/10.1016/S0022-3476(95)70548-1.
American Academy of Pediatrics Committee on Infectious Diseases, Committee on Fetus and Newborn. Prevention of respiratory syncytial virus infections: Indications for the use of palivizumab and update on the use of RSV-IGIV. Pediatrics 1998;102(5):1211-6. https://doi.org/10.1542/peds.102.5.1211.
American Academy of Pediatrics Committee on Infectious Diseases, Committee on Fetus and Newborn. Revised indications for the use of palivizumab and respiratory syncytial virus immune globulin intravenous for the prevention of respiratory syncytial virus infections. Pediatrics 2003;112(6 pt 1):1442-6.
Committee on Infectious Diseases. From the American Academy of Pediatrics: Policy statements - Modified recommendations for use of palivizumab for prevention of respiratory syncytial virus infections. Pediatrics 2009;124(6):1694-701.
https://doi.org/10.1542/peds.2009-2345.
American Academy of Pediatrics Committee on Infectious Diseases, American Academy of Pediatrics Bronchiolitis Guidelines Committee. Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics 2014;134(2):415-20. https://doi.org/10.1542/peds.2014-1665.
Heljic S, Maksic H, Begic H, Skokic F, Glamuzina D, Bozic T, et al. Palivizumab prophylaxis of RSV infections in Bosnia and Herzegovina. J Pediatr Neonat Individual Med 2016;5(1):e050129.
Rietveld E, Vergouwe Y, Steyerberg EW, Huysman MW, de Groot R, Moll HA, et al. Hospitalization for respiratory syncytial virus infection in young children: Development of a clinical prediction rule. Pediatr Infect Dis J 2006;25(3):201-7. https://doi.org/10.1097/01.inf.0000202135.24485.f8.
Joffe S, Escobar GJ, Black SB, Armstrong MA, Lieu TA. Rehospitalization for respiratory syncytial virus among premature infants. Pediatrics 1999;104(4 Pt 1):894-9. https://doi.org/10.1542/peds.104.4.894.
Trefny P, Stricker T, Baerlocher C, Sennhauser FH. Family history of atopy and clinical course of RSV infection in ambulatory and hospitalized infants. Pediatr Pulmonol 2000;30(4):302-6. https://doi.org/10.1002/1099-0496(200010)30:4<302::AID-PPUL5>3.0.CO;2-R.
Wu CC, Chen RF, Kuo HC. Different implications of paternal and maternal atopy for perinatal IgE production and asthma development. Clin Dev Immunol 2012;2012:132142. https://doi.org/10.1155/2012/132142.
Rodríguez DA, Rodríguez-Martínez CE, Cárdenas AC, Quilaguy IE, Mayorga LY, Falla LM, et al. Predictors of severity and mortality in children hospitalized with respiratory syncytial virus infection in a tropical region. Pediatr Pulmonol 2014;49(3):269-76. https://doi.org/10.1002/ppul.22781.
Borchers AT, Chang C, Gershwin ME, Gershwin LJ. Respiratory syncytial virus - A comprehensive review. Clin Rev Allergy Immunol 2013;45(3):331-79. https://doi.org/10.1007/s12016-013-8368-9.
Saha S, Pandey BG, Choudekar A, Krishnan A, Gerber SI, Rai SK, et al. Evaluation of case definitions for estimation of respiratory syncytial virus associated hospitalizations among children in a rural community of northern India. J Glob Health 2015;5(2):010419. https://doi.org/10.7189/jogh.05.020419.
Durani Y, Friedman MJ, Attia MW. Clinical predictors of respiratory syncytial virus infection in children. Pediatr Int 2008;50(3):352-5.
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2018-01-02
Published 2018-08-01









