Safety of once- or twice-daily dosing of non-vitamin K antagonist oral anticoagulants (NOACs) in patients with nonvalvular atrial fibrillation: A NOAC-TR study
DOI:
https://doi.org/10.17305/bjbms.2017.2279Keywords:
Daily dosing, bleeding, medication adherence, non-vitamin K antagonist oral anticoagulants, self-report, NOACs, nonvalvular atrial fibrillation, NVAFAbstract
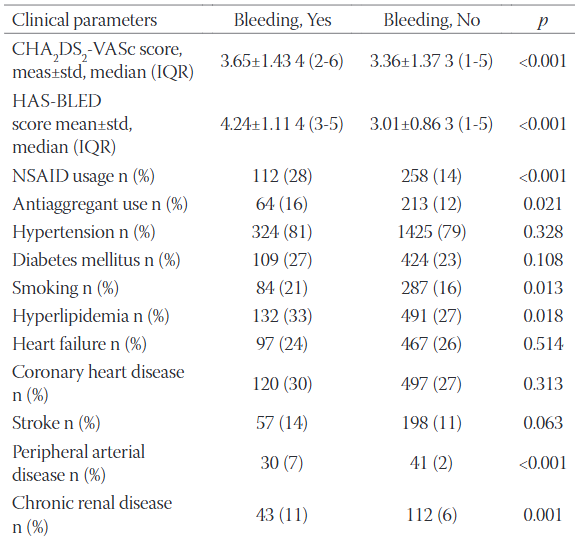
Once-daily dosing of non-vitamin K antagonist oral anticoagulants (NOACs) may increase patient adherence to treatment but may also be associated with a higher risk of bleeding. In this study, we investigated the adherence to once- or twice-daily dosing of NOACs and the risk of bleeding in nonvalvular atrial fibrillation (NVAF) patients. This multicenter cross-sectional study, conducted between 1 September 2015 and 28 February 2016, included 2214 patients receiving NOACs for at least 3 months, due to NVAF. Patients receiving once-daily or twice-daily NOAC doses were 1:1 propensity score matched for baseline demographic characteristics and the presence of other diseases. The medication adherence was assessed by the 8-item Morisky Medication Adherence Scale. Risk factors were investigated in relation to minor and major bleeding. The mean age of patients was 71 ± 10 years, and 53% of the patients were women. The medication adherence was lower in patients receiving twice-daily NOAC doses compared to once-daily-dose group (47% versus 53%, p = 0.001), and there was no difference between the groups in terms of minor (15% versus 16%, p = 0.292) and major bleeding (3% versus 3%, p = 0.796). Independent risk factors for bleeding were non-adherence to medication (OR: 1.62, 95% CI: 1.23–2.14, p = 0.001), presence of 3 or more other diseases (OR: 10.3, 95% CI: 5.3–20.3, p < 0.001), and HAS-BLED (Hypertension, Abnormal renal and liver function, Stroke, Bleeding, Labile INR, Elderly, Drugs or alcohol) score (OR: 4.84, 95% CI: 4.04–5.8, p < 0.001). In summary, the once-daily dose of NOACs was associated with increased patient adherence to medication, while it was not associated with bleeding complications.
Citations
Downloads
References
Nieuwlaat R, Connolly BJ, Hubers LM, Cuddy SM, Eikelboom JW, Yusuf S, et al. Quality of individual INR control and the risk of stroke and bleeding events in atrial fibrillation patients: A nested case control analysis of the ACTIVE W study. Thromb Res 2012;129(6):715-9. https://doi.org/10.1016/j.thromres.2011.08.024.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. RE-LY steering committee and ınvestigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2010;361(12):1139-51. https://doi.org/10.1056/NEJMoa0905561.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 2011;365(10):883-91. https://doi.org/10.1056/NEJMoa1009638.
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2011;365(11):981-92. https://doi.org/10.1056/NEJMoa1107039.
Schulman S, Kearon C, Kakkar AK, Mismetti P, Schellong S, Eriksson H, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med 2009;361(24):2342-52. https://doi.org/10.1056/NEJMoa0906598.
Landman G, Gans R. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med 2011;364(36):1178. https://doi.org/10.1056/NEJMc1100734.
Shameem R, Ansell J. Disadvantages of VKA and requirements for novel anticoagulants. Best Pract Res Clin Haematol 2013;26(2):103-14. https://doi.org/10.1016/j.beha.2013.07.009.
Emren SV, Senöz O, Bilgin M, Beton O, Aslan A, Taskin U, et al. Drug adherence in patients with nonvalvular atrial fibrillation taking non-Vitamin K antagonist oral anticoagulants in Turkey. Clin Appl Thromb Hemost 2018;24(3):525-31. https://doi.org/1076029617693940.
Laliberté F, Nelson WW, Lefebvre P, Schein JR, Rondeau-Leclaire J, Duh MS. Impact of daily dosing frequency on adherence to chronic medications among nonvalvular atrial fibrillation patients. Adv Ther 2012;29(8):675-90.
https://doi.org/10.1007/s12325-012-0040-x.
McHorney CA, Crivera C, Laliberté F, Nelson WW, Germain G, Bookhart B, et al. Adherence to non-VKA oral anticoagulant medications based on the pharmacy quality alliance measure. Curr Med Res Opin 2015;31(12):1-16. https://doi.org/10.1185/03007995.2015.1096242.
Coleman CI, Tangirala M, Evers T. Treatment persistence and discontinuation with rivaroxaban, dabigatran, and warfarin for stroke prevention in patients with non-valvular atrial fibrillation in the United States. PLoS One 2016;11(6):e0157769. https://doi.org/10.1371/journal.pone.0157769.
Nelson WW, Song X, Coleman CI, Thomson E, Smith DM, Damaraju CV, et al. Medication persistence and discontinuation of rivaroxaban versus warfarin among patients with non-valvular atrial fibrillation. Curr Med Res Opin 2014;30(12):2461-9.
https://doi.org/10.1185/03007995.2014.933577.
Graham DJ, Reichman ME, Wernecke M, Hsueh YH, Izem R, Southworth MR, et al. Stroke, bleeding, and mortality risks in elderly medicare beneficiaries treated with dabigatran or rivaroxaban for nonvalvular atrial fibrillation. JAMA Intern Med 2016;176(11):1662-71.
https://doi.org/10.1001/jamainternmed.2016.5954.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10(5):348-54.
https://doi.org/10.1111/j.1751-7176.2008.07572.x.
Pan F, Chernew ME, Fendrick AM. Impact of fixed-dose combination drugs on adherence to prescription medications. J Gen Intern Med 2008;23(5):611-4. https://doi.org/10.1007/s11606-008-0544-x.
Alberts MJ, Peacock WF, Fields LE, Bunz TJ, Nguyen E, Milentijevic D, et al. Association between once- and twice-daily direct oral anticoagulant adherence in nonvalvular atrial fibrillation patients and rates of ischemic stroke. Int J Cardiol 2016;215:11-3.
https://doi.org/10.1016/j.ijcard.2016.03.212.
Forslund T, Wettermark B, Hjemdahl P. Comparison of treatment persistence with different oral anticoagulants in patients with atrial fibrillation. Eur J Clin Pharmacol 2016;72(3):329-38. https://doi.org/10.1007/s00228-015-1983-z.
Brown JD, Shewale AR, Talbert JC. Adherence to rivaroxaban, dabigatran, and apixaban for stroke prevention in ıncident, treatment-naïve nonvalvular atrial fibrillation. J Manage Care Spec Pharm 2016;22(11):1319-29. https://doi.org/10.18553/jmcp.2016.22.11.1319.
Castellucci LA, Shaw J, van der Salm K, Erkens P, Le Gal G, Petrcich W, et al. Self-reported adherence to anticoagulation and its determinants using the Morisky medication adherence scale. Thromb Res 2015;136(4):727-31. https://doi.org/10.1016/j.thromres.2015.07.007.
Luger S, Hohmann C, Niemann D, Kraft P, Gunreben I, Neumann-Haefelin T, et al. Adherence to oral anticoagulant therapy in secondary stroke prevention-impact of the novel oral anticoagulants. Patient Prefer Adherence 2015;23(9):1695-705. https://doi.org/10.2147/PPA.S88994.
Heidbuchel H, Verhamme P, Alings M, Antz M, Hacke W, Oldgren J, et al. European heart rhythm association practical guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation. Europace 2013;15(5):625-51. https://doi.org/10.1093/europace/eut083.
Vrijens B, Heidbuchel H. Non-Vitamin K antagonist oral anticoagulants: Considerations on once-versus. Twice-daily regimens and their potential impact on medication adherence. Europace 2015;17(4):514-23. https://doi.org/10.1093/europace/euu311.
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2018 Bosnian Journal of Basic Medical Sciences

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2017-08-31
Published 2018-05-20









