Pethidine efficacy in achieving the ultrasound-guided oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy: A prospective study
DOI:
https://doi.org/10.17305/bjbms.2016.1647Keywords:
Pethidine, oblique subcostal transversus abdominis plane block, laparoscopic cholecystectomy, analgesiaAbstract
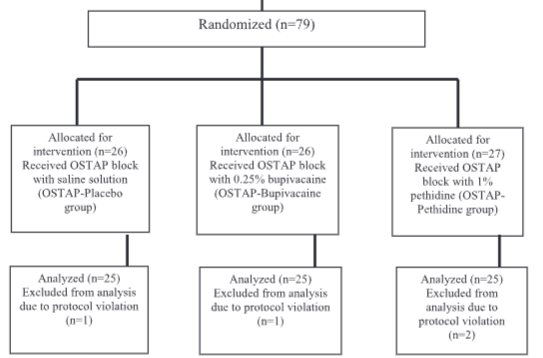
Pethidine is a synthetic opioid with local anesthetic properties. Our goal was to evaluate the analgesic efficacy of pethidine for achieving the ultrasound-guided oblique subcostal transversus abdominis plane (OSTAP) block in laparoscopic cholecystectomy. This prospective, double-blind study included 79 patients of physical status I and II according to American Society of Anesthesiologists, scheduled for elective laparoscopic cholecystectomy. The patients were randomly allocated into three groups, depending on the drug used to achieve preoperative bilateral OSTAP block: 1) OSTAP-Placebo (treated with normal saline); 2) OSTAP-Bupivacaine (treated with 0.25% bupivacaine); and 3) OSTAP-Pethidine (treated with 1% pethidine). The efficacy of pethidine in achieving the OSTAP block was analyzed using visual analog scale (VAS), intraoperative opioid dose, opioid consumption in post anesthesia care unit, and opioid consumption in the first 24 postoperative hours. The pain scores assessed by VAS at 0, 2, 4, 6, 12, and 24 hours were significantly lower in OSTAP-Pethidine than in OSTAP-Placebo group (p < 0.001). The mean intraoperative opioid consumption was significantly lower in OSTAP-Pethidine compared to OSTAP-Placebo group (150 versus 400 mg, p < 0.001), as well as the mean opioid consumption in the first 24 hours (20.4 versus 78 mg, p < 0.001). Comparing VAS assessment between OSTAP-Bupivacaine and OSTAP-Pethidine groups, statistically significant differences were observed only for the immediate postoperative pain assessment (0 hours), where lower values were observed in OSTAP-Pethidine group (p = 0.004). There were no statistically significant differences in the incidence of postoperative nausea and vomiting (p = 0.131) between the groups. The use of 1% pethidine can be an alternative to 0.25% bupivacaine in achieving OSTAP block for laparoscopic cholecystectomy.
Citations
Downloads
References
Bisgaard T. Analgesic treatment after laparoscopic cholecystectomy: A critical assessment of the evidence. Anesthesiology 2006;104(4):835-46. http://dx.doi.org/10.1097/00000542-200604000-00030.
Ekstein P, Szold A, Sagie B, Werbin N, Klausner JM, Weinbroum AA. Laparoscopic surgery may be associated with severe pain and high analgesia requirements in the immediate postoperative period. Ann Surg 2006;243(1):41-6. http://dx.doi.org/10.1097/01.sla.0000193806.81428.6f.
Kum CK, Wong CW, Goh PM, Ti TK. Comparative study of pain level and analgesic requirement after laparoscopic and open cholecystectomy. Surg Laparosc Endosc 1994;4(2):139-41.
Tihan D, Totoz T, Tokocin M, Ercan G, Koc TC, Vartanoglu T, et al. Efficacy of laparoscopic transversus abdominis plane block for elective laparoscopic cholecystectomy in elderly patients. Bosn J Basic Med Sci 2016;16(2):139-44. http://dx.doi.org/10.17305/bjbms.2016.841.
Hong D, Flood P, Diaz G. The side effects of morphine and hydromorphone patient - controlled analgesia. Anesth Analg 2008;107(4):1384-9. http://dx.doi.org/10.1213/ane.0b013e3181823efb.
Erol DD, Yilmaz S, Polat C, Arikan Y. Efficacy of thoracic epidural analgesia for laparoscopic cholecystectomy. Adv Ther 2008;25(1):45-52. http://dx.doi.org/10.1007/s12325-008-0005-2.
Boddy AP, Mehta S, Rhodes M. The effect of intraperitoneal local anesthesia in laparoscopic cholecystectomy-a systemic review and meta-analysis. Anesth Analg 2006;103(3):682-8. http://dx.doi.org/10.1213/01.ane.0000226268.06279.5a.
Rafi AN. Abdominal field block: A new approach via the lumbar triangle. Anaesthesia 2001;56(10):1024-6.
http://dx.doi.org/10.1046/j.1365-2044.2001.02279-40.x.
McDonnell JG, O'Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: A prospective randomized controlled trial. Anesth Analg 2007;104(1):193-7. http://dx.doi.org/10.1213/01.ane.0000250223.49963.0f.
Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care 2007;35(4):616-7.
El-Dawlatly AA, Turkistani A, Kettner SC, Machata AM, Delvi MB, Thallaj A, et al. Ultrasound-guided transversus abdominis plane block: Description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth 2009;102(6):763-7. http://dx.doi.org/10.1093/bja/aep067.
Ra YS, Kim CH, Lee GY, Han JI. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol 2010;58(4):362-8. http://dx.doi.org/10.4097/kjae.2010.58.4.362.
Ripollés J, Mezquita SM, Abad A, Calvo J. Analgesic efficacy of the ultrasound-guided blockade of the transversus abdominis plane - a systematic review. [Article in Portuguese] Rev Bras Anestesiol 2015;65(4):255-80. http://dx.doi.org/10.1016/j.bjan.2013.10.014.
Beyazova M, Babacan A, Bilir E, Akçabay M, Kaya K, Baysal AI. Perineural pethidine: Effects of different doses on nerve conduction. Eur J Anaesthesiol 1993; 10(5):353-6.
Armstrong PJ, Morton C, Nimmo F. Pethidine has a local anaesthetic action on peripheral nerves in vivo. Addition to prilocaine 0.25% for intravenous regional anaesthesia in volunteers. Anaesthesia 1993;48(5):382-6.
http://dx.doi.org/10.1111/j.1365-2044.1993.tb07008.x.
Cunha TM, Souza GR, Domingues AC, Carreira EU, Lotufo CM, Funez MI, et al. Stimulation of peripheral Kappa opioid receptors inhibits inflammatory hyperalgesia via activation of the PI3Kg/AKT/nNOS/NO signaling pathway. Mol Pain 2012;8:10. http://dx.doi.org/10.1186/1744-8069-8-10.
Wagner LE 2nd, Eaton M, Sabnis SS, Gingrich KJ. Meperidine and lidocaine block of recombinant voltage-dependent Na+ channels: Evidence that meperidine is a local anesthetic. Anesthesiology 1999;91(5):1481-90.
http://dx.doi.org/10.1097/00000542-199911000-00042.
Stein C. The control of pain in peripheral tissue by opioids. N Engl J Med 1995; 332(25):1685-90. http://dx.doi.org/10.1056/NEJM199506223322506.
Wood A. New method of treating neuralgia by the direct application of opiates to the painful points. Edinburgh Med Surg J 1955;82:265.
Hong JY, Lee IH. Comparison of the effects of intrathecal morphine and pethidine on shivering after Caesarean delivery under combined-spinal epidural anaesthesia. Anaesthesia 2005;60(12):1168-72.
http://dx.doi.org/10.1111/j.1365-2044.2005.04158.x.
Hashemi SJ, Soltani H, Heidari SM, Rezakohanfekr M. Preemptive analgesia with intra-articular pethidine reduces pain after arthroscopic knee surgery. Adv Biomed Res 2013;2:9. http://dx.doi.org/10.4103/2277-9175.107971.
Jabalameli M, Safavi M, Honarmand A, Saryazdi H, Moradi D, Kashefi P. The comparison of intraincisional injection tramadol, pethidine and bupivacaine on postcesarean section pain relief under spinal anesthesia. Adv Biomed Res 2012;1:53. http://dx.doi.org/10.4103/2277-9175.100165.
Petersen PL, Stjernholm P, Kristiansen VB, Torup H, Hansen EG, Mitchell AU, et al. The beneficial effect of transversus abdominis plane block after laparoscopic cholecystectomy in day-case surgery: A randomized clinical trial. Anesth Analg 2012; 115(3):527-33. http://dx.doi.org/10.1213/ane.0b013e318261f16e.
Tolchard S, Davies R, Martindale S. Efficacy of the subcostal transversus abdominis plane block in laparoscopic cholecystectomy: Comparison with conventional port-site infiltration. J Anaesthesiol Clin Pharmacol 2012;28(3):339-43. http://dx.doi.org/10.4103/0970-9185.98331.
Söderlund A, Boreus LO, Westman L, Engström B, Valentin A, Ekblom A. A comparison of 50, 100 and 200 mg of intra-articular pethidine during knee joint surgery, a controlled study with evidence for local demethylation to norpethidine. Pain 1999;80(1-2):229-38.
http://dx.doi.org/10.1016/S0304-3959(98)00207-3.
Onutu AH, Iacob IM, Todor A, Lucaciu DO, Acalovschi I. Wound infiltration with 1% pethidine provides an opioid-sparing effect after uncemented total hip arthroplasty: A prospective randomized study. Rom J Anesth Int Care 2012;19(1):5-12.
Matkap E, Bedirli N, Akkaya T, Gümüş H. Preincisional local infiltration of tramadol at the trocar site versus intravenous tramadol for pain control after laparoscopic cholecystectomy. J Clin Anesth 2011;23(3):197-201.
http://dx.doi.org/10.1016/j.jclinane.2010.08.010.
Siddiqui MR, Sajid MS, Uncles DR, Cheek L, Baig MK. A meta-analysis on the clinical effectiveness of transversus abdominis plane block. J Clin Anesth 2011;23(1): 7-14. http://dx.doi.org/10.1016/j.jclinane.2010.05.008.
Yu N, Long X, Lujan-Hernandez JR, Succar J, Xin X, Wang X. Transversus abdominis-plane block versus local anesthetic wound infiltration in lower abdominal surgery: A systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol 2014;14:121. http://dx.doi.org/10.1186/1471-2253-14-121.
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2016 Bosnian Journal of Basic Medical Sciences

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2016-10-03
Published 2017-02-21









