Advancing ICU mortality prediction in community-acquired pneumonia: Combining fibrinogen-to-albumin ratio, CT severity score, PSI, and CURB-65
DOI:
https://doi.org/10.17305/bb.2025.12127Keywords:
Community-acquired pneumonia, CAP, fibrinogen-to-albumin ratio, FAR, CT severity score, CT-SS, Pneumonia Severity Index, PSIAbstract
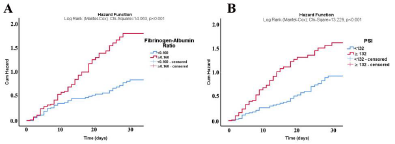
Community-acquired pneumonia (CAP) is a leading cause of ICU admissions, with significant morbidity and mortality. Traditional risk stratification tools, such as CURB-65, the pneumonia severity index (PSI), and computed tomography severity scores (CT-SS) are widely used for prognosis but could be improved by incorporating novel biomarkers. This retrospective study evaluated the fibrinogen-to-albumin ratio (FAR) as an additional predictor of 30-day mortality in ICU patients with CAP. A total of 158 CAP patients admitted to a tertiary care ICU were included. Baseline data encompassed demographic, clinical, laboratory, and radiological parameters, including FAR, CURB-65, PSI, and CT-SS. Logistic regression and receiver operating characteristic curve (ROC) analyses were conducted to assess mortality predictors. The 30-day mortality rate was 70.88% (112/158). Higher FAR, PSI, CURB-65, CT-SS, and lactate levels were independently associated with increased mortality (P < 0.05). FAR demonstrated strong discriminatory power (area under the receiver operating characteristic [AUROC]: 0.704) and significantly improved the predictive accuracy of established models. Adding FAR to PSI increased the AUROC from 0.705 to 0.791 (P = 0.009), while combining FAR, CT-SS, and PSI yielded the highest predictive accuracy (AUROC: 0.844, P = 0.032). These findings suggest that FAR, which reflects both inflammation and nutritional status, complements traditional risk assessment tools by providing a dynamic perspective. Integrating FAR into existing models enhances the identification of high-risk patients, enabling timely interventions and more efficient resource allocation in the ICU.
Citations
Downloads
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Ece Unal Cetin, Ozge Kurtkulagi, Fatih Kamis, Murat Das, Esen Simsek, Adil Ugur Cetin, Yavuz Beyazit

This work is licensed under a Creative Commons Attribution 4.0 International License.