Microsatellite instability status predicts response to anti-PD-1/PD-L1 therapy regardless the histotype: A comment on recent advances
DOI:
https://doi.org/10.17305/bjbms.2017.2366Keywords:
microsatellite instability, anti-PD-1, PD-L1, therapyAbstract
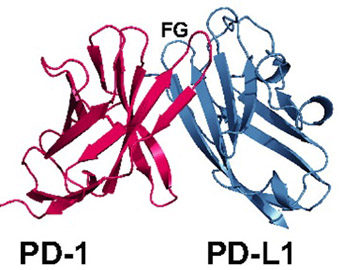
It is well-known that somatic mutations resulting in increased number of neoantigens (“immunogenic antigens”) may enhance anti-tumor immune cell reaction. Also, high tumor mutation burden (load) [TML] is associated with improved response, durable clinical benefits and better outcome if a cancer is treated with immune check point inhibitors [anti-programmed cell death protein 1/programmed death-ligand 1 (anti-PD-1/PD-L1) drugs] [1]. A subset of colorectal carcinomas (CRC) and other cancers characterized by mismatch repair deficiency (MMR) and/or microsatellite instability high (MSI-H) profiles may be particularly sensitive to the PD-1/PD-L1 blockade with immune check point inhibitors due to the common PD-L1/PD-L1 expression [2-9]. Several therapeutic antibodies inhibiting either PD-1 (nivolumab, pembrolizumab) or PD-L1 (MPDL3280A, Medi4736, BMS-936559) have been developed and approved for the treatment of various malignancies including malignant melanoma, non-small cell lung carcinoma, renal cell carcinoma, bladder carcinoma, Merkel cell carcinoma, and classical Hodgkin lymphoma [10].
A pivotal phase 2 study by Le et al. [11] highlighted the importance of mismatch-repair status in prediction of the clinical benefit of immune checkpoint blockade with pembrolizumab (anti-PD-1 drug) [11]. The study included 41 patients with progressive cancers of both CRC and non-colorectal origins and known MSI status. For CRC patients, the objective response rate and progression-free survival rate were 40% and 78%, respectively for mismatch repair-deficient tumors and 0% and 11% for mismatch repair-proficient CRCs.
A novel study by Le et al. [12] (ClinicalTrials.gov number, NCT01876511) represents an extended analysis on the efficacy of PD-1 blockade in patients with advanced mismatch repair-deficient cancers. The study included 86 patients with 12 different histologic cancer subtypes and proved mismatch repair-deficiency status assessed by either polymerase chain reaction (PCR) or immunohistochemistry. The data presented in this study indicate objective radiographic responses in 53% of patients while complete responses were achieved in 21% of patients. Based on this and previous data, on May 23, 2017, the U.S. Food and Drug Administration (FDA) granted accelerated approval to anti-PD-L1 drug pembrolizumab (KEYTRUDA®, Merck & Co.) for adult and pediatric patients with unresectable/metastatic MSI-H/MMR deficient solid tumors (regardless the histotype) that have progressed following prior treatment and without satisfactory alternative treatment modalities. The approval also covered MSI-H CRC patients who progressed following treatment with a classic cytotoxic therapy (fluoropyrimidine, oxaliplatin, and irinotecan).
Taken together, these results revolutionize the cancer treatment paradigm as for the first time the cancer treatment was based solely on the molecular characteristics of cancer (in this case microsatellite instability/MSI/ status) regardless the tumor morphology (histotype). This appears to be “the FDA’s first tissue/site-agnostic approval”.
Certainly, there are still ongoing but unresolved issues regarding these treatments including other merging predictive biomarkers (optimization of PD-L1 and PD-1 evaluation, e.g. tumor versus immune cell expression; cutoffs for positivity; selection of detection antibodies), tumor mutational load and the tumor neoantigen heterogeneity/specificity [13-15]. Further studies should also elucidate the mechanisms of recently described resistance to immune checkpoint inhibitors [16-18].
Citations
Downloads
References
Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 2015;348(6230):124-8. https://doi.org/10.1126/science.aaa1348.
Lee V, Murphy A, Le DT, Diaz LA, Jr. Mismatch repair deficiency and response to immune checkpoint blockade. Oncologist 2016;21(10):1200-11. https://doi.org/10.1634/theoncologist.2016-0046.
Lau E. Mismatch repair deficiency predicts benefit of anti-PD-1 therapy. Lancet Oncol 2015;16(7):e319. https://doi.org/10.1016/S1470-2045(15)00031-5.
Czink E, Kloor M, Goeppert B, Froehling S, Uhrig S, Weber TF, et al. Successful immune checkpoint blockade in a patient with advanced stage microsatellite unstable biliary tract cancer. Cold Spring Harb Mol Case Stud. 2017. [Epub ahead of print]. DOI: 10.1101/mcs.a001974.
Castro MP, Goldstein N. Mismatch repair deficiency associated with complete remission to combination programmed cell death ligand immune therapy in a patient with sporadic urothelial carcinoma: Immunotheranostic considerations. J Immunother Cancer 2015;3:58. https://doi.org/10.1186/s40425-015-0104-y.
Gatalica Z, Snyder C, Maney T, Ghazalpour A, Holterman DA, Xiao N, et al. Programmed cell death 1 (PD-1) and its ligand (PD-L1) in common cancers and their correlation with molecular cancer type. Cancer Epidemiol Biomarkers Prev 2014;23(12):2965-70. https://doi.org/10.1158/1055-9965.EPI-14-0654.
Gatalica Z, Vranic S, Xiu J, Swensen J, Reddy S. High microsatellite instability (MSI-H) colorectal carcinoma: A brief review of predictive biomarkers in the era of personalized medicine. Fam Cancer 2016;15(3):405-12. https://doi.org/10.1007/s10689-016-9884-6.
Llosa NJ, Cruise M, Tam A, Wicks EC, Hechenbleikner EM, Taube JM, et al. The vigorous immune microenvironment of microsatellite instable colon cancer is balanced by multiple counter-inhibitory checkpoints. Cancer Discov 2015;5(1):43-51.
https://doi.org/10.1158/2159-8290.CD-14-0863.
Overman MJ, McDermott R, Leach JL, Lonardi S, Lenz HJ, Morse MA, et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): An open-label, multicentre, phase 2 study. Lancet Oncol 2017. [Epub ahead of print]. https://doi.org/10.1016/S1470-2045(17)30422-9.
Sunshine J, Taube JM. PD-1/PD-L1 inhibitors. Curr Opin Pharmacol 2015;23:32-8. https://doi.org/10.1016/j.coph.2015.05.011.
Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med 2015;372(26):2509-20. https://doi.org/10.1056/NEJMoa1500596.
Le DT, Durham JN, Smith KN, Wang H, Bartlett BR, Aulakh LK, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science 2017;357(6349):409-13. https://doi.org/10.1126/science.aan6733.
McGranahan N, Furness AJ, Rosenthal R, Ramskov S, Lyngaa R, Saini SK, et al. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science 2016;351(6280):1463-9. https://doi.org/10.1126/science.aaf1490.
Gubin MM, Zhang X, Schuster H, Caron E, Ward JP, Noguchi T, et al. Checkpoint blockade cancer immunotherapy targets tumour-specific mutant antigens. Nature 2014;515(7528):577-81. https://doi.org/10.1038/nature13988.
Chalmers ZR, Connelly CF, Fabrizio D, Gay L, Ali SM, Ennis R, et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med 2017;9(1):34. https://doi.org/10.1186/s13073-017-0424-2.
Anagnostou V, Smith KN, Forde PM, Niknafs N, Bhattacharya R, White J, et al. Evolution of neoantigen landscape during immune checkpoint blockade in non-small cell lung cancer. Cancer Discov 2017;7(3):264-76. https://doi.org/10.1158/2159-8290.CD-16-0828.
Wang Q, Wu X. Primary and acquired resistance to PD-1/PD-L1 blockade in cancer treatment. Int Immunopharmacol 2017;46:210-9. https://doi.org/10.1016/j.intimp.2017.03.015.
Shin DS, Zaretsky JM, Escuin-Ordinas H, Garcia-Diaz A, Hu-Lieskovan S, Kalbasi A, et al. Primary resistance to PD-1 blockade mediated by JAK1/2 mutations. Cancer Discov 2017;7(2):188-201. https://doi.org/10.1158/2159-8290.CD-16-1223.
Downloads
Additional Files
Published
How to Cite
Accepted 2017-08-16
Published 2017-08-20