Comparison of local infiltration and epidural analgesia for postoperative pain control in total knee arthroplasty and total hip arthroplasty: A systematic review and meta-analysis
DOI:
https://doi.org/10.17305/bjbms.2016.1072Keywords:
Total knee arthroplasty, total hip arthroplasty, local infiltration, epidural analgesia, meta-analysisAbstract
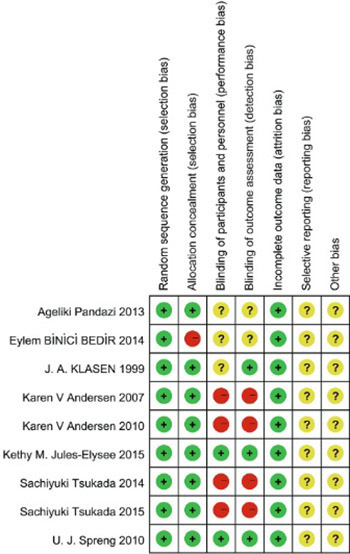
Pain management after total knee arthroplasty (TKA) and total hip arthroplasty should permit early mobilization with minimal pain. Local infiltration analgesia (LIA) is a new popular method for decreasing postoperative pain. The goal of this meta-analysis is to evaluate the efficacy of LIA in comparison with epidural analgesia. A literature search was performed in PubMed, EMBASE, the OVID database, Web of Science, and the Cochrane Library databases. The risk of bias was assessed using the Cochrane collaboration tool. Outcomes of interest included visual analog scale score, range of flexion, length of stay, and complications. Nine trials involving 537 patients met the inclusion criteria. LIA provides better pain relief and larger range of motion in TKA patients compared to epidural analgesia at the late postoperative period. No significant difference was observed in regard to the length of stay and complications. The current evidence shows that the use of local infiltration is effective for postoperative pain management in TKA patients. More high-quality randomized controlled trials with long-term follow-up are required for examining the long-term efficacy and safety of local infiltration.
Citations
Downloads
References
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780-5. http://dx.doi.org/10.2106/JBJS.F.00222.
Nussenzveig TC. Pain management after total joint replacement and its impact on patient outcomes. AORN J. 1999;70(6):1060-2. http://dx.doi.org/10.1016/s0001-2092(06)62213-8.
Capdevila X, Barthelet Y, Biboulet P, Ryckwaert Y, Rubenovitch J, d'Athis F. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999;91(1):8-15. http://dx.doi.org/10.1097/00000542-199907000-00006.
Choi PT, Bhandari M, Scott J, Douketis J. Epidural analgesia for pain relief following hip or knee replacement. Cochrane Database Syst Rev. 2003;3:CD003071. http://dx.doi.org/10.1002/14651858.cd003071.
Tang R, Evans H, Chaput A, Kim C. Multimodal analgesia for hip arthroplasty. Orthop Clin North Am. 2009;40(3):377-87. http://dx.doi.org/10.1016/j.ocl.2009.04.001.
Bianconi M, Ferraro L, Traina GC, Zanoli G, Antonelli T, Guberti A, et al. Pharmacokinetics and efficacy of ropivacaine continuous wound instillation after joint replacement surgery. Br J Anaesth 2003;91(6):830-5. http://dx.doi.org/10.1093/bja/aeg277.
Kerr DR, Kohan L. Local infiltration analgesia: A technique for the control of acute postoperative pain following knee and hip surgery: A case study of 325 patients. Acta Orthop. 2008;79(2):174-83. http://dx.doi.org/10.1080/17453670710014950.
Teng Y, Jiang J, Chen S, Zhao L, Cui Z, Khan MS, et al. Periarticular multimodal drug injection in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1949-57. http://dx.doi.org/10.1007/s00167-013-2566-0.
Jiang J, Teng Y, Fan Z, Khan MS, Cui Z, Xia Y. The efficacy of periarticular multimodal drug injection for postoperative pain management in total knee or hip arthroplasty. J Arthroplasty. 2013;28(10):1882-7.
http://dx.doi.org/10.1016/j.arth.2013.06.031.
Andersen KV, Bak M, Christensen BV, Harazuk J, Pedersen NA, Søballe K. A randomized, controlled trial comparing local infiltration analgesia with epidural infusion for total knee arthroplasty. Acta Orthop. 2010;81(5):606-10. http://dx.doi.org/10.3109/17453674.2010.519165.
Spreng UJ, Dahl V, Hjall A, Fagerland MW, Ræder J. High-volume local infiltration analgesia combined with intravenous or local ketorolac morphine compared with epidural analgesia after total knee arthroplasty. Br J Anaesth. 2010;105(5):675-82. http://dx.doi.org/10.1093/bja/aeq232.
Klasen JA, Opitz SA, Melzer C, Thiel A, Hempelmann G. Intraarticular, epidural, and intravenous analgesia after total knee arthroplasty. Acta Anaesthesiol Scand. 1999;43(10):1021-6. http://dx.doi.org/10.1034/j.1399-6576.1999.431009.x.
Tsukada S, Wakui M, Hoshino A. Pain control after simultaneous bilateral total knee arthroplasty: A randomized controlled trial comparing periarticular injection and epidural analgesia. J Bone Joint Surg Am. 2015;97(5):367-73. http://dx.doi.org/10.2106/JBJS.N.00373.
Jules-Elysee KM, Goon AK, Westrich GH, Padgett DE, Mayman DJ, Ranawat AS, et al. Patient-controlled epidural analgesia or multimodal pain regimen with periarticular injection after total hip arthroplasty: A randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am. 2015;97(10):789-98. http://dx.doi.org/10.2106/JBJS.N.00698.
Pandazi A, Kanellopoulos I, Kalimeris K, Batistaki C, Nikolakopoulos N, Matsota P, et al. Periarticular infiltration for pain relief after total hip arthroplasty: A comparison with epidural and PCA analgesia. Arch Orthop Trauma Surg. 2013;133(11):1607-12.
http://dx.doi.org/10.1007/s00402-013-1849-8.
Tsukada S, Wakui M, Hoshino A. Postoperative epidural analgesia compared with intraoperative periarticular injection for pain control following total knee arthroplasty under spinal anesthesia: A randomized controlled trial. J Bone Joint Surg Am. 2014;96(17):1433-8. http://dx.doi.org/10.2106/JBJS.M.01098.
Andersen KV, Pfeiffer-Jensen M, Haraldsted V, Søballe K. Reduced hospital stay and narcotic consumption, and improved mobilization with local and intraarticular infiltration after hip arthroplasty: A randomized clinical trial of an intraarticular technique versus epidural infusion in 80 patients. Acta Orthop. 2007;78(2):180-6. http://dx.doi.org/10.1080/17453670710013654.
Binici Bedir E, Kurtulmus T, Basyigit S, Bakir U, Saglam N, Saka G. A comparison of epidural analgesia and local infiltration analgesia methods in pain control following total knee arthroplasty. Acta Orthop Traumatol Turc. 2014;48(1):73-9. http://dx.doi.org/10.3944/AOTT.2014.3256.
Mullaji A, Kanna R, Shetty GM, Chavda V, Singh DP. Efficacy of periarticular injection of bupivacaine, fentanyl, and methylprednisolone in total knee arthroplasty: A prospective, randomized trial. J Arthroplasty. 2010;25(6):851-7. http://dx.doi.org/10.1016/j.arth.2009.09.007.
Starks I, Frost A, Wall P, Lim J. Is a fracture of the transverse process of L5 a predictor of pelvic fracture instability? J Bone Joint Surg Br. 2011;93(7):967-9. http://dx.doi.org/10.1302/0301-620X.93B7.26772.
Liu SS, Richman JM, Thirlby RC, Wu CL. Efficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: A quantitative and qualitative systematic review of randomized controlled trials. J Am Coll Surg. 2006;203(6):914-32. http://dx.doi.org/10.1016/j.jamcollsurg.2006.08.007.
Vendittoli PA, Makinen P, Drolet P, Lavigne M, Fallaha M, Guertin MC, et al. A multimodal analgesia protocol for total knee arthroplasty. A randomized, controlled study. J Bone Joint Surg Am. 2006;88(2):282-9. http://dx.doi.org/10.2106/JBJS.E.00173.
Mather LE. The acute toxicity of local anesthetics. Expert Opin Drug Metab Toxicol. 2010;6(11):1313-32.
http://dx.doi.org/10.1517/17425255.2010.514265.
Zhang S, Wang F, Lu ZD, Li YP, Zhang L, Jin QH. Effect of single-injection versus continuous local infiltration analgesia after total knee arthroplasty: A randomized, double-blind, placebo-controlled study. J Int Med Res. 2011;39(4):1369-80. http://dx.doi.org/10.1177/147323001103900423.
Andersen LØ, Kristensen BB, Husted H, Otte KS, Kehlet H. Local anesthetics after total knee arthroplasty: Intraarticular or extraarticular administration? A randomized, double-blind, placebo-controlled study. Acta Orthop. 2008;79(6):800-5. http://dx.doi.org/10.1080/17453670810016885.
Perret M, Fletcher P, Firth L, Yates P. Comparison of patient outcomes in periarticular and intraarticular local anaesthetic infiltration techniques in total knee arthroplasty. J Orthop Surg Res. 2015;10:119. http://dx.doi.org/10.1186/s13018-015-0249-x.
Nakai T, Tamaki M, Nakamura T, Nakai T, Onishi A, Hashimoto K. Controlling pain after total knee arthroplasty using a multimodal protocol with local periarticular injections. J Orthop. 2013;10(2):92-4. http://dx.doi.org/10.1016/j.jor.2013.02.001.
Downloads
Additional Files
Published
How to Cite
Accepted 2016-03-08
Published 2016-11-10









